Overview
Melancholic depression can bring about profound sadness and a sense of hopelessness that many may struggle to articulate. It often includes anhedonia, psychomotor changes, and a range of physical and emotional symptoms that can significantly impact daily life. Recognizing these symptoms is crucial for early intervention, as it opens the door to a supportive path forward.
In addition to acknowledging these challenges, it’s essential to explore the various treatment options available.
- Medication
- Psychotherapy
- Lifestyle changes
can all play a role in recovery. Effective management often requires a multifaceted approach, tailored to individual needs, ensuring that each person receives the care that resonates with them.
We understand that navigating these feelings can be daunting, but remember, you are not alone. Seeking help is a courageous step towards healing. We’re here for you, ready to support you on this journey. Your comfort is our priority, and together, we can work towards a brighter tomorrow.
Introduction
In a world where emotional struggles often go unnoticed, melancholic depression emerges as a profound mental health challenge that affects countless individuals, particularly seniors. This condition is marked by overwhelming sadness and a stark loss of interest in activities that once brought joy. It is a severe subtype of major depressive disorder, encompassing a range of debilitating symptoms. Persistent feelings of worthlessness, along with significant changes in sleep and appetite, are common experiences for those affected. Understanding melancholic depression is crucial for timely intervention and support.
As awareness of this condition grows, so does the need for effective treatment strategies and robust support systems. These resources empower those affected to reclaim their lives. We want you to know that you are not alone in this journey. This article delves into the multifaceted nature of melancholic depression, exploring its symptoms, causes, treatment options, and the vital role of support networks in fostering recovery. Together, we can navigate this path towards healing and hope.
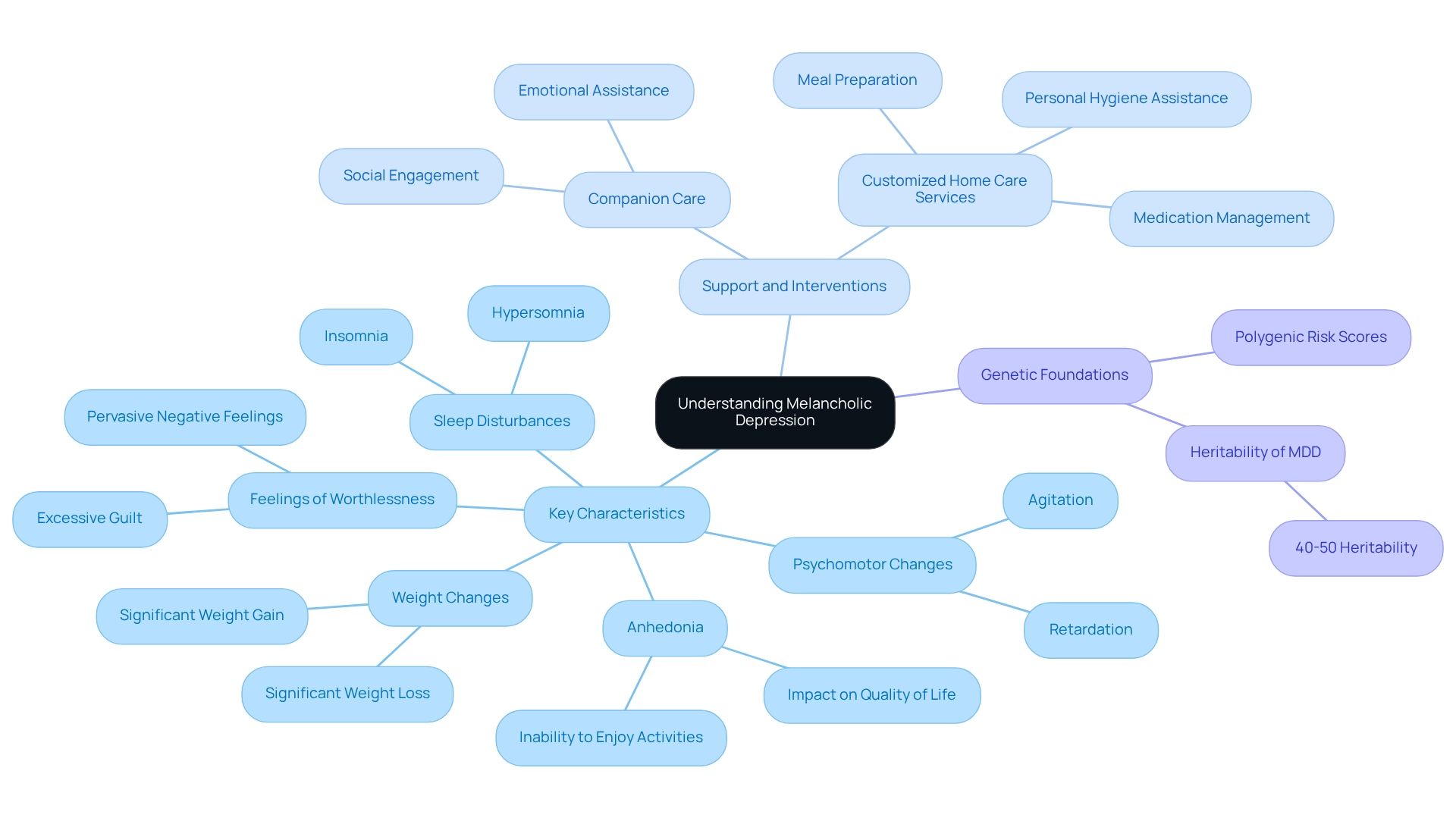
Defining Melancholic Depression: Key Characteristics and Symptoms
Melancholic depression, often referred to as melancholia, is a serious subtype of major depressive disorder (MDD) characterized by profound sorrow and a significant loss of interest or enjoyment in nearly all activities. This condition encompasses a range of physical and psychological symptoms that can deeply affect daily life, especially for seniors. Recognizing these symptoms is vital for identifying mood disorders in oneself or others, particularly among seniors who may face unique challenges.
Key characteristics of mood disorders include:
- Anhedonia: A marked inability to derive pleasure from activities that were once enjoyable, significantly impacting quality of life.
- Psychomotor changes: Individuals may experience agitation or retardation, presenting as noticeable restlessness or physical slowing, complicating their ability to engage in daily tasks.
- Weight changes: Fluctuations in weight, whether significant loss or gain, often linked to alterations in appetite, further complicating the individual’s condition.
- Sleep disturbances: Insomnia or hypersomnia (excessive sleeping) disrupt normal sleep patterns and contribute to overall fatigue.
- Feelings of worthlessness or excessive guilt: These pervasive feelings can intensify the negative state, making it crucial to address them in treatment.
Signs that indicate a loved one may need companion or sitter services include social isolation, difficulty with daily tasks, and safety concerns. Companion care services from Best Care Nurses Registry can play a crucial role in enhancing the quality of life for seniors experiencing these symptoms. By offering social engagement and emotional assistance, caregivers can help reduce feelings of loneliness and sadness, contributing to improved mental well-being.
Furthermore, customized home care services can assist with everyday activities that may become burdensome due to sadness, such as meal preparation, medication management, and personal hygiene. These services can be tailored to meet the specific needs and schedules of seniors, ensuring flexibility and convenience. This assistance not only helps preserve autonomy but also guarantees a more secure living space, lowering the chances of accidents and health issues.
Recent studies have highlighted the genetic foundations of sadness, indicating that polygenic risk scores (PRS) for MDD are linked to specific clinical subtypes and characteristics. Research involving 1,149 MDD patients showed that higher PRS for MDD and loneliness were associated with traits of melancholic depression, suggesting a distinct genetic profile for this subtype. Notably, the estimated twin-based heritability of MDD is approximately 40-50%, indicating a significant genetic component.
Dr. Dold emphasizes that it is feasible to forecast the diagnosis of mood disorders and their clinical typology from immunometabolic markers and lifestyle habits, utilizing machine learning methods. Mental health professionals stress the importance of early identification and intervention, as effective treatment can significantly improve outcomes for those affected. As the occurrence of mental and substance use disorders continues to rise, representing 15% of the overall disease burden in various areas, awareness and education about conditions such as severe sadness are more essential than ever. We’re here for you, and your comfort is our priority.
Recognizing the Symptoms: Emotional and Physical Signs of Melancholic Depression
Symptoms of sorrowful mood disorders can be categorized into emotional and physical signs, each playing a critical role in understanding this condition.
Emotional Symptoms:
- Persistent Sadness: Many individuals experience a profound and unshakable sadness that can feel overwhelming, significantly impacting daily life. This persistent feeling can be incredibly challenging to navigate.
- Loss of Interest: A marked disinterest in activities that were once enjoyable often leads to social withdrawal and isolation, making it harder to connect with loved ones.
- Feelings of Despair: A pervasive sense of hopelessness about the future is common, which can exacerbate feelings of worthlessness and anxiety, leaving many feeling trapped.
Physical Symptoms:
- Fatigue: A constant feeling of tiredness that does not improve with rest is prevalent among those suffering from melancholic depression. This fatigue can lead to decreased productivity and motivation, adding to the burden of daily life.
- Sleep Disturbances: Many individuals face difficulties in falling asleep, staying asleep, or may experience excessive sleeping. These disturbances disrupt daily routines and can deepen feelings of despair.
- Changes in Appetite: Significant weight loss or gain can occur due to altered eating habits, reflecting the emotional turmoil experienced during this time.
- Psychomotor Agitation or Retardation: This can manifest as noticeable restlessness or slowed physical movements, affecting the ability to engage in everyday activities, which can be frustrating and disheartening.
Identifying these symptoms is essential for prompt intervention and assistance. Recent studies suggest that sad mood disorders are more common among women, with a female-to-male occurrence rate ratio of 2.13. Furthermore, case studies have shown that persistent sadness and fatigue are common real-life examples of this condition, highlighting the need for awareness and understanding.
As co-author Mats Bogren notes, “[insert quote here].” By recognizing both emotional and physical signs, caregivers and family members can provide better support to those affected, ensuring they receive the necessary care and intervention. Additionally, the study titled “Machine Learning in Major Depression Classification” illustrates how symptoms manifest and are classified, providing a practical context for the discussion. Remember, you’re not alone in this journey; we’re here for you, and your comfort is our priority.
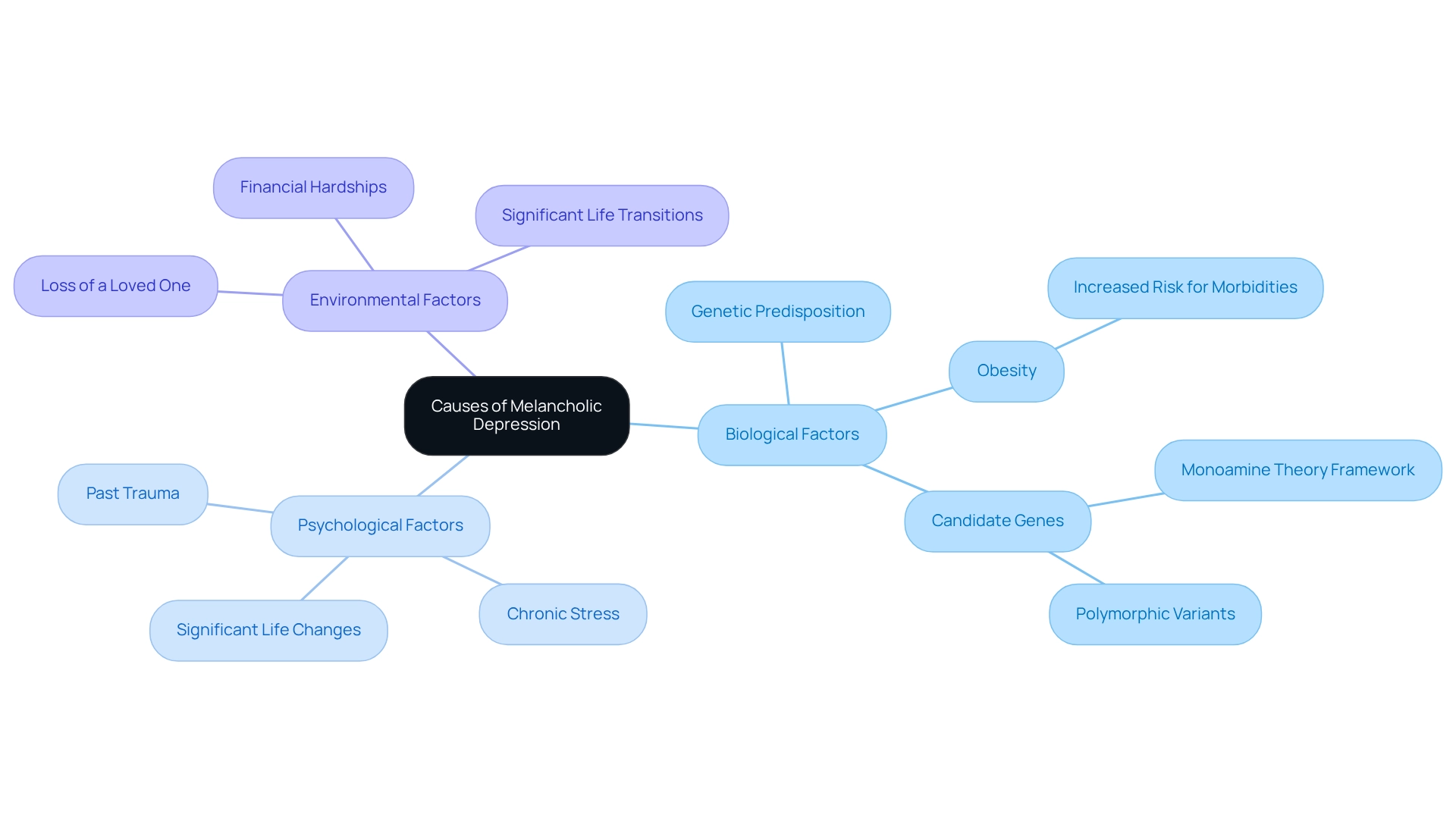
Exploring the Causes: What Triggers Melancholic Depression?
Melancholic sadness can arise from a complex interplay of various factors, and it’s important to understand these to foster a sense of hope and healing.
Biological Factors: Genetic predisposition plays a significant role in the likelihood of developing melancholic sadness. Research indicates that individuals with a family background of mood disorders face an increased risk. Studies have even identified specific genes linked to the onset of depressive conditions. Notably, meta-analyses have revealed connections between polymorphic variants of genes not typically associated with this condition, underscoring the intricate biological foundations at play. Additionally, obesity can heighten the risk for other ailments related to late-life sadness, including pain syndromes and disability, which can further complicate the health of seniors.
Psychological Factors: It’s essential to recognize that psychological triggers—such as past trauma, chronic stress, and significant life changes—are crucial in the onset of despair. These factors can disrupt emotional stability, leading to depressive episodes. Experts emphasize that understanding these psychological triggers is vital for effective management and treatment of melancholic depression. As Philip E. Mosley, Chief Scientific Advisor, notes, addressing these triggers is key to better managing anxiety and depression.
Environmental Factors: Situational stressors, including the loss of a loved one, financial hardships, or significant life transitions, can intensify feelings of sadness and hopelessness. Real-life instances illustrate how these ecological factors can lead to the emergence of sadness, particularly in vulnerable groups. Recent studies have shown no notable connections between facial and brain state dynamics and anxiety symptoms among individuals experiencing deep sadness, highlighting the complexity of these conditions. Acknowledging these multifaceted causes is essential for developing effective treatment plans and preventive strategies, ultimately enhancing the quality of life for those affected by severe mood disorders. Remember, you are not alone in this journey; support and understanding are always available.
Treatment Approaches: From Medication to Therapy for Melancholic Depression
Effective treatment for depressive disorders typically involves a multifaceted approach that combines various strategies designed to support you on your journey toward healing.
- Medications: Antidepressants can play a crucial role in managing depressive conditions. Research indicates that tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) are often more effective for depressive traits than selective serotonin reuptake inhibitors (SSRIs). A recent meta-analysis by Laura C. Morgan highlights the comparative benefits and harms of these medications, underscoring the importance of personalized treatment plans, especially for elderly patients who may have unique health considerations.
- Psychotherapy: Cognitive Behavioral Therapy (CBT) is a widely recognized therapeutic modality that assists individuals in processing their emotions and developing effective coping strategies. Current statistics show that psychotherapy can lead to significant improvements in depressive symptoms, with many patients reporting enhanced quality of life following treatment. This is particularly relevant for older adults, who may face additional emotional challenges.
- Electroconvulsive Therapy (ECT): For severe instances of profound mood disorders, especially when other treatments have shown little success, ECT may be considered. This approach has demonstrated efficacy in rapidly alleviating symptoms in patients who do not respond to conventional therapies, including older adults who may require more immediate intervention.
- Lifestyle Changes: Incorporating regular physical activity, maintaining a balanced diet, and ensuring adequate sleep are essential components of a holistic treatment plan. These lifestyle changes can greatly improve overall wellness and aid in symptom relief, which is vital for seniors striving to maintain their independence.
A thorough treatment strategy customized to your specific needs is crucial for effectively managing melancholic depression. Insights from therapists emphasize the importance of ongoing assessment and adjustment of treatment strategies to optimize outcomes for patients. Furthermore, a study revealed that factors like sadness, PTSD, and TBI significantly affect veterans, highlighting the necessity for targeted interventions.
The VA is also funding a project to study the genomics of major depressive disorder, aiming to personalize antidepressant prescriptions based on genetic information. This could pave the way for more effective treatments tailored specifically for the elderly population. Remember, you are not alone in this journey; we’re here for you, and your comfort is our priority.
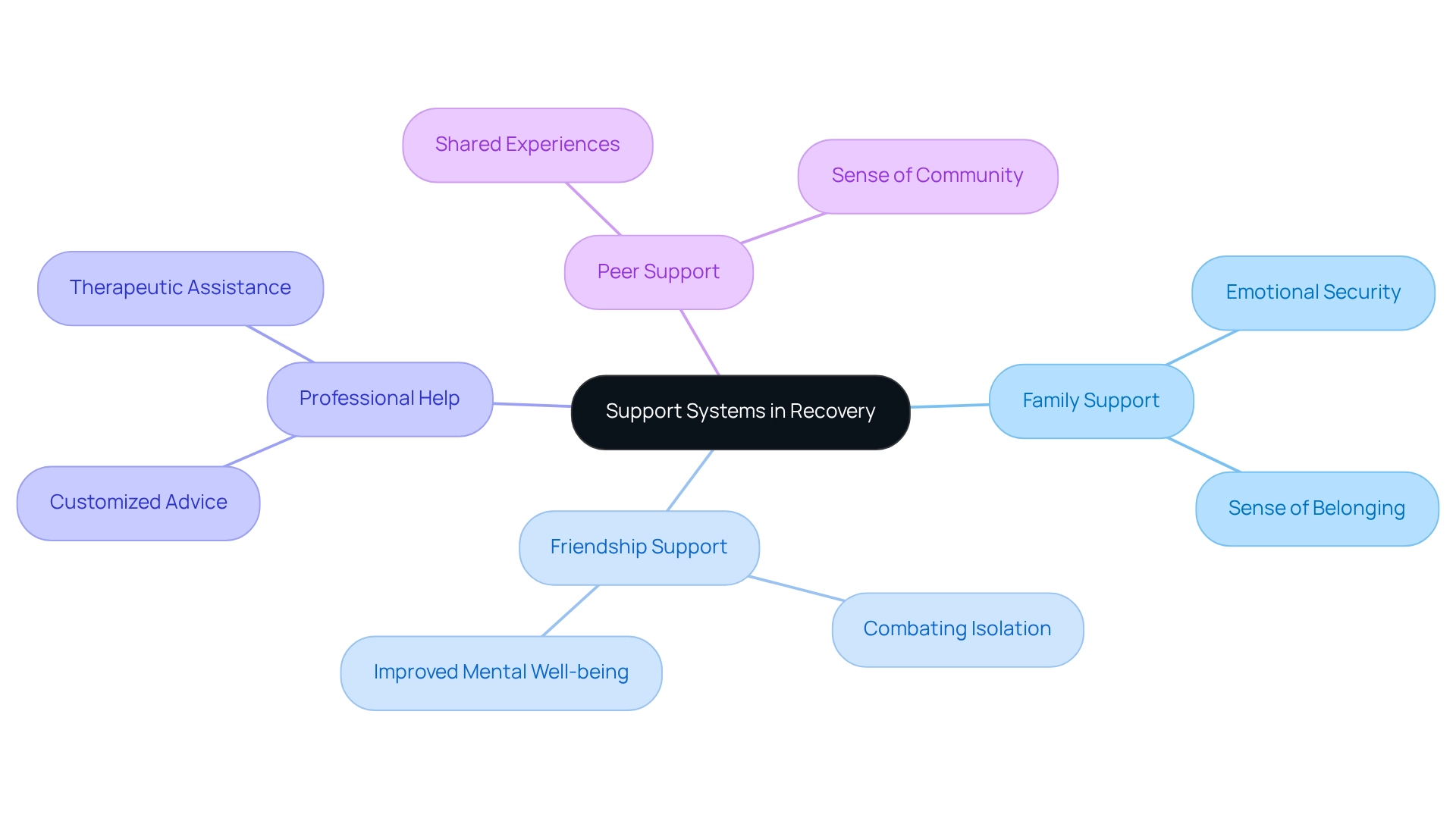
The Role of Support Systems: How Relationships Impact Recovery
Support systems are essential in the recovery journey for individuals grappling with melancholic depression. The encouragement and understanding provided by family members can create a profound sense of security and belonging, which is crucial for emotional healing. Research suggests that assistance from close relationships has a strong negative correlation with feelings of despair (b = 0.48, p = 0.000), emphasizing the significance of family involvement in mental health recovery.
Caryn Pearson, an analyst with the Health Statistics Division, emphasizes that ‘the role of family support cannot be overstated in the recovery process.’ Friendships also play a crucial role in combating feelings of isolation and loneliness that often accompany melancholic depression. Sustaining social ties can greatly improve emotional strength, as people who interact with friends report better mental well-being results.
The existence of encouraging friends can serve as a shield against the emotional impact of depression, promoting a feeling of community and shared experience.
In addition to familial and social assistance, professional help is crucial. Interacting with mental wellness experts offers individuals customized advice and therapeutic assistance, equipping them with coping techniques to handle their symptoms efficiently. The incorporation of professional care into one’s assistance network can result in more organized recovery pathways.
Furthermore, groups provide another layer of help, enabling individuals to exchange their experiences and coping strategies with others encountering similar challenges. These groups can foster a sense of belonging and understanding, reinforcing the idea that no one is alone in their struggles. The economic consequences of ignoring mental wellness are substantial, with severe mental disorders leading to $193.2 billion in lost income within the U.S. economy annually, highlighting the importance of efficient assistance frameworks.
Moreover, participation in activities enhancing wellbeing can be encouraged by these assistance frameworks. ‘Information shows that numerous people who take part in social and physical activities report better mental health, implying that encouraging such involvement can be a successful approach for boosting overall wellbeing.
In general, developing and sustaining a strong network is essential for the efficient handling and recovery from melancholic depression. The interplay of family, friendships, professional help, and peer support creates a comprehensive network that can significantly enhance an individual’s journey toward mental wellness.
Self-Care Strategies: Empowering Individuals to Cope with Melancholic Depression
Implementing self-care strategies can significantly aid in managing melancholic depression.
- Establish a Routine: Creating a daily schedule provides structure and a sense of normalcy, which is essential for emotional stability. We understand that maintaining a consistent routine can help you cope with the unpredictability of your feelings.
- Engage in Physical Activity: Regular exercise is crucial, as it releases endorphins that improve mood. Research shows that individuals who participate in moderate to intense physical activity experience significant decreases in symptoms of low mood and anxiety. Staying active is not just beneficial; it’s a fundamental method for addressing low mood and anxiety, as highlighted by public wellness guidelines.
- Practice Mindfulness and Relaxation Techniques: Activities such as meditation, yoga, or deep breathing exercises can significantly reduce stress and enhance emotional well-being. Mindfulness methods have been shown to assist individuals in handling their thoughts and emotions more efficiently, resulting in improved mental well-being outcomes. For instance, a study found that the average depression score for meditators was 30.51, lower than the cut-off point of 36, while non-meditators scored 40.82. This illustrates the potential benefits of mindfulness practices.
- Maintain a Healthy Diet: A balanced diet abundant in nutrients promotes overall well-being and can positively influence mood. Nutritional studies suggest that certain foods can influence brain chemistry, thereby affecting emotional states.
- Prioritize Sleep Hygiene: Ensuring adequate and quality sleep is crucial for mental health. Poor sleep can worsen symptoms of low mood, making it essential to establish good sleep practices.
As Park, a nurse, reflects, “With the prolonged COVID-19, I have one more task added to my already full to-do list. I need to take care of my mind that is about to collapse. I sit comfortably with my eyes closed and try to untangle my feelings of anxiety, frustration, resentment, regrets, and failures.
When sutra copying, I become kind, supportive, and understanding toward myself. This is why I continue copying the sutra.” By integrating these approaches, you can strengthen your ability to manage melancholic depression more effectively, fostering resilience and enhancing your overall quality of life. Remember, we’re here for you, and your comfort is our priority.
Debunking Myths: Common Misconceptions About Melancholic Depression
Numerous myths about melancholic depression persist, often obstructing effective understanding and treatment of this serious condition.
- Myth 1: Melancholic depression is merely a phase or a sign of weakness.
Fact: Melancholic depression is a significant mental health disorder that necessitates appropriate treatment. It is not a reflection of personal strength or character. - Myth 2: Individuals experiencing feelings of deep sadness can simply ‘snap out of it.’
Fact: Recovery typically involves a multifaceted approach, including therapy, medication, and robust support systems. The complexity of melancholic depression indicates that it cannot be overcome through willpower alone. - Myth 3: Only older individuals encounter sorrowful states.
Fact: This condition can lead to melancholic depression, impacting individuals across all age groups. In fact, the highest occurrence rate of mood disorder takes place in individuals aged 40 to 49, emphasizing that it is not limited to the elderly.
Tackling these misunderstandings is essential for fostering a more supportive atmosphere for those impacted by sadness. A recent report indicated that 18.4% of U.S. adults have been diagnosed with a mood disorder at some point, with significant variability across states. This highlights the importance of acknowledging and comprehending the prevalence of melancholic depression among different demographics.
As Louise Brådvik from Lund University notes, “Grasping the subtleties of sadness is crucial for effective therapy and assistance.” By dispelling these myths, we can motivate more individuals to seek the assistance they require and promote a culture of understanding and encouragement. Remember, you are not alone in this journey, and reaching out for help is a brave and important step.
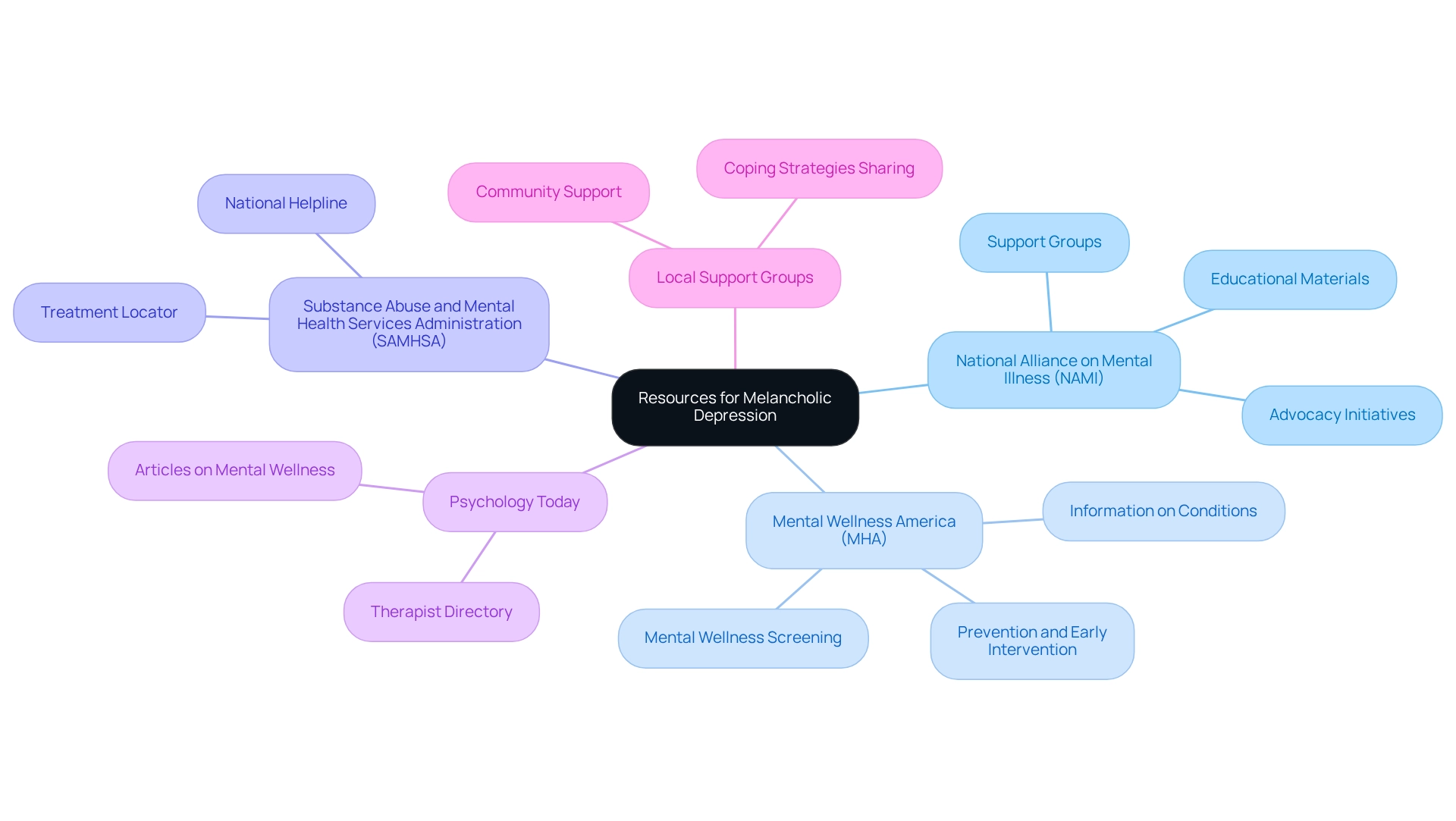
Further Resources: Where to Find Help and Information on Melancholic Depression
For individuals seeking further information and support regarding melancholic depression, a variety of resources are available to assist in managing this condition effectively:
- National Alliance on Mental Illness (NAMI): This organization offers a wealth of educational materials, support groups, and advocacy initiatives aimed at individuals facing mental health challenges. NAMI’s programs are designed to foster understanding and provide a community for those affected by mental illness.
- Mental Wellness America (MHA): MHA offers vital resources for mental wellness screening, along with extensive information and support customized to different mental wellness conditions. Their focus on prevention and early intervention is crucial for the effective management of melancholic depression.
- Substance Abuse and Mental Health Services Administration (SAMHSA): SAMHSA provides a national helpline and a treatment locator, facilitating access for individuals to locate mental wellness services in their area. This accessibility is crucial, particularly given that service utilization rates for adjustment disorders rose by 6.4% during the pandemic, emphasizing a rising demand for assistance.
- Psychology Today: This platform offers a therapist directory and a variety of articles on mental wellness subjects, giving individuals choices to locate professional assistance tailored to their requirements.
- Local Support Groups: Many communities host support groups specifically for individuals dealing with depression. These groups can be invaluable for sharing experiences and coping strategies. Checking local listings can uncover options that may be beneficial.
In addition to these resources, it is important to acknowledge the ongoing challenges in obtaining mental care. A study on access to mental wellness services showed that even in states with high rankings for treatment availability, over 40% of adults with mental disorders did not obtain care. This underscores the necessity of utilizing available resources and advocating for better access to mental health services.
As Dr. Amarachi Eke-Okoro emphasizes, finding the right assistance is crucial for effectively managing melancholic depression. Engaging with these resources can provide the necessary support and information to navigate this challenging condition. Furthermore, it is critical to acknowledge the alarming increase in suicide rates, which rose by approximately 36% between 2000 and 2022, with 1.6 million adults making a suicide attempt in 2022.
This statistic highlights the severity of mental health issues and the importance of seeking help. Remember, you are not alone in this journey; reaching out for support is a vital step towards healing.
Conclusion
Understanding melancholic depression is essential for recognizing its profound impact on individuals, particularly seniors. This condition presents a unique set of challenges, characterized by intense sadness, anhedonia, and significant changes in sleep and appetite. The symptoms can manifest both emotionally and physically, leading to a debilitating experience that necessitates timely intervention and support.
Effective treatment strategies encompass a holistic approach, combining medication, psychotherapy, and lifestyle modifications. The importance of personalized care cannot be overstated, especially for the elderly population who may face additional health complexities. Furthermore, the role of robust support systems—comprising family, friends, and mental health professionals—is crucial in facilitating recovery and fostering resilience.
Addressing the myths surrounding melancholic depression is vital for creating a supportive environment that encourages individuals to seek help. By dispelling misconceptions and promoting awareness, we can cultivate a culture of understanding that ultimately leads to better mental health outcomes.
In conclusion, navigating the complexities of melancholic depression requires a multifaceted strategy that integrates effective treatment, strong support networks, and self-care practices. It is imperative to empower individuals with the knowledge and resources needed to manage their mental health, paving the way for healing and hope. Together, we can work towards reducing the stigma and enhancing the quality of life for those affected by this challenging condition. Remember, we’re here for you, and your comfort is our priority.
Frequently Asked Questions
What is melancholic depression?
Melancholic depression, or melancholia, is a serious subtype of major depressive disorder characterized by profound sorrow and a significant loss of interest or enjoyment in nearly all activities, impacting daily life, especially for seniors.
What are the key characteristics of mood disorders?
Key characteristics include anhedonia (inability to derive pleasure), psychomotor changes (agitation or retardation), weight changes (fluctuations in appetite), sleep disturbances (insomnia or hypersomnia), and feelings of worthlessness or excessive guilt.
How can one identify if a loved one may need companion or sitter services?
Signs that indicate a loved one may need such services include social isolation, difficulty with daily tasks, and safety concerns.
What role do companion care services play for seniors experiencing melancholic depression?
Companion care services can enhance the quality of life by providing social engagement and emotional assistance, helping to reduce feelings of loneliness and sadness.
What types of customized home care services are available for seniors?
Customized home care services can include assistance with daily activities such as meal preparation, medication management, and personal hygiene, tailored to meet specific needs and schedules.
What recent research has been conducted regarding the genetic foundations of melancholic depression?
Recent studies have shown that polygenic risk scores for major depressive disorder are linked to specific clinical subtypes, indicating a distinct genetic profile for melancholic depression, with an estimated heritability of 40-50%.
How can machine learning methods help in diagnosing mood disorders?
Machine learning methods can forecast the diagnosis and clinical typology of mood disorders from immunometabolic markers and lifestyle habits, emphasizing the importance of early identification and intervention.
Why is awareness and education about mood disorders important?
Awareness and education are essential as the occurrence of mental and substance use disorders continues to rise, representing a significant portion of the overall disease burden, highlighting the need for understanding conditions like melancholic depression.











