Overview
Dehydration in the elderly can be a serious concern, often stemming from factors like:
- Decreased thirst sensation
- Chronic illnesses
- Certain medications
- Mobility issues
- Environmental influences
These challenges can lead to significant health risks that worry many families.
Understanding these causes is crucial, as it allows us to take proactive steps to protect our loved ones. Implementing effective prevention strategies, such as:
- Encouraging regular fluid intake
- Monitoring hydration status
can make a meaningful difference in safeguarding the well-being of older adults.
We recognize how important it is to ensure that our seniors stay hydrated, as this not only enhances their quality of life but also reduces the complications associated with dehydration. Remember, your comfort and health are our priorities, and we’re here for you every step of the way.
Introduction
In a world where hydration is often overlooked, we must turn our attention to a silent yet critical health crisis affecting our elderly loved ones: dehydration. This condition impacts up to 30% of older adults and can lead to serious complications, including cognitive decline and increased hospitalization rates.
It’s essential for caregivers and families to understand the multifaceted causes of dehydration and recognize its symptoms.
How can we implement proactive strategies to safeguard the health and well-being of seniors, ensuring they remain hydrated and vibrant in their golden years? Together, we can make a difference.
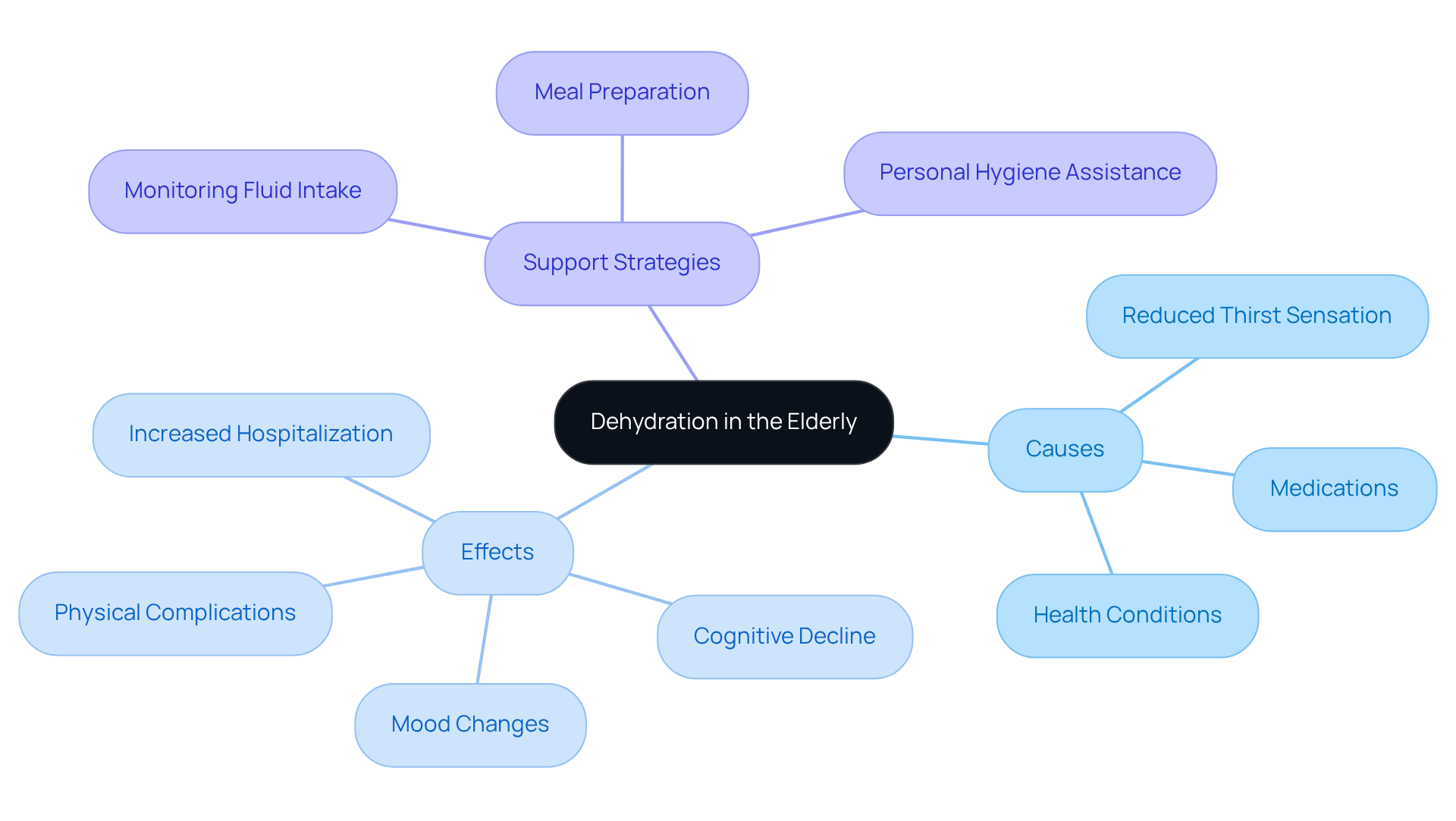
Define Dehydration and Its Impact on the Elderly
Dehydration occurs when the body loses more fluids than it takes in, resulting in insufficient water and electrolytes essential for normal bodily functions. This condition is particularly concerning for elderly individuals, who may face heightened risks of dehydration due to factors such as a reduced thirst sensation, medications that promote fluid loss, and various underlying health conditions. Recent studies indicate that dehydration in elderly individuals affects 20% to 30% of older adults, often leading to serious complications like urinary tract infections, kidney stones, and increased hospitalization rates. Did you know that insufficient hydration can double the mortality rate among stroke patients? This underscores the critical importance of maintaining proper fluid levels for health outcomes.
Furthermore, chronic fluid deficiency is associated with adverse effects, including cognitive decline, mood changes, and physical complications such as falls and fractures. Understanding the consequences of fluid loss is vital for safeguarding the well-being and quality of life of older adults to prevent dehydration in elderly. This is where the compassionate support of CNA/HHA caregiver services becomes invaluable. These dedicated caregivers provide personalized care, helping to monitor fluid intake, assist with meal preparation to ensure proper nutrition, and support personal hygiene—essential elements in preventing dehydration in elderly individuals.
By ensuring that seniors receive the necessary assistance, caregivers can significantly enhance their quality of life and independence. Together, we can make proactive measures to ensure adequate hydration more achievable. Remember, your comfort and well-being are our top priorities, and we’re here for you every step of the way.
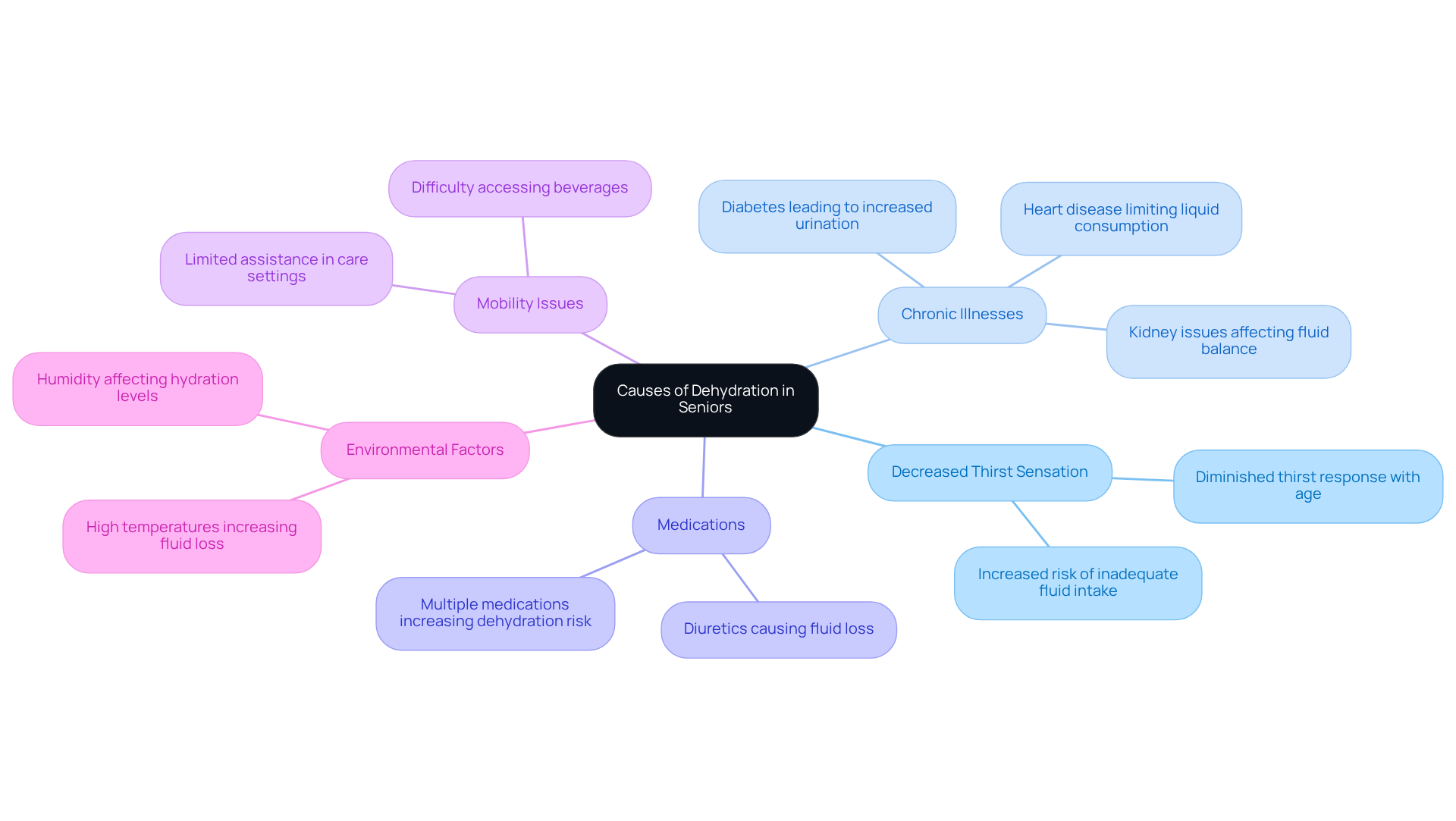
Identify Causes of Dehydration in Seniors
Several factors contribute to dehydration in elderly individuals, and understanding these can make a significant difference in their well-being.
-
Decreased Thirst Sensation: As we age, our body’s thirst response often diminishes, leading to inadequate fluid intake. Studies show that dehydration in elderly individuals may occur due to a notable decline in their thirst sensation, making it less likely for them to drink enough water. This can be concerning, as staying hydrated is vital for health.
-
Chronic Illnesses: Conditions such as diabetes, heart disease, and kidney issues can elevate moisture loss or reduce water intake. For instance, diabetes can lead to increased urination, while heart disease may limit liquid consumption due to dietary restrictions. Recognizing these challenges is essential for caregivers to provide the necessary support and prevent dehydration in elderly.
-
Medications: Certain medications, particularly diuretics, can cause increased urination and loss of bodily fluids. This is a common issue among older adults, who often take multiple medications for various health conditions. Understanding how these medications affect dehydration in elderly can help in managing their intake.
-
Mobility Issues: Seniors with restricted mobility may struggle to access beverages regularly. This challenge can be even more pronounced in long-term care settings, where the risk of dehydration in elderly individuals may not always be adequately addressed due to limited assistance. Caregivers from Best Care Nurses Registry can play a vital role in ensuring that seniors have consistent access to beverages. By setting reminders to drink water and incorporating hydration into meal planning, caregivers can make a real difference.
-
Environmental Factors: High temperatures or elevated humidity can worsen moisture loss through sweating. During the summer months, the risk of losing body moisture increases, especially for elderly individuals who might not adjust their beverage consumption accordingly.
Recognizing these causes is crucial for caregivers to implement effective hydration strategies to prevent dehydration in elderly individuals, ensuring that seniors maintain adequate fluid levels and overall health. Furthermore, understanding the physiological processes that lead to fluid loss, such as the activation of the renin-angiotensin-aldosterone system and the reduced sensitivity of the thirst mechanism in older adults, can provide deeper insights into this issue. Moreover, dehydration in elderly individuals can hinder cognitive function, as studies show that even mild fluid deficiency can negatively impact memory and concentration.
By collaborating with a caregiver from Best Care Nurses Registry, families can ensure that their loved ones receive the personalized support they need to stay hydrated and healthy. Remember, your comfort is our priority, and we’re here for you.
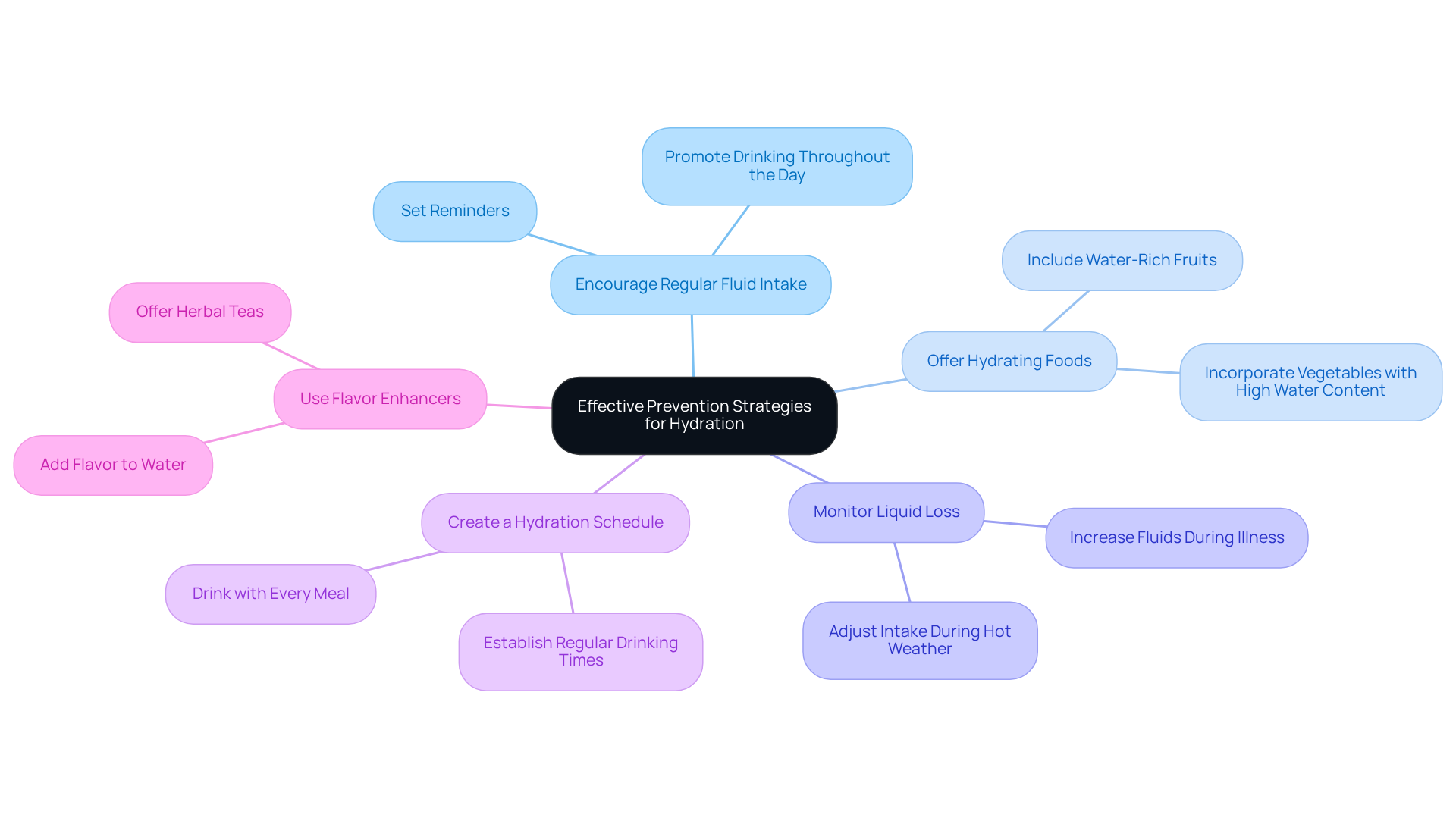
Implement Effective Prevention Strategies for Hydration
To prevent dehydration in elderly individuals, it’s important to consider some supportive strategies that can make a significant difference:
- Encourage Regular Fluid Intake: Gently remind seniors to drink water throughout the day, even if they don’t feel thirsty. Setting reminders can be incredibly helpful, as older adults often experience a diminished thirst sensation. It’s crucial to prompt them to hydrate regularly, ensuring they feel cared for and supported.
- Offer Hydrating Foods: Incorporate fruits and vegetables with high water content, such as watermelon, cucumbers, and oranges, into their diet. These nourishing foods not only provide moisture but also essential nutrients that promote overall well-being, making meals more enjoyable and beneficial.
- Monitor Liquid Loss: Keep an eye on factors that may increase liquid loss, such as hot weather or illness, and adjust liquid intake accordingly. For instance, during heat waves, it’s essential to encourage higher beverage intake to counteract the effects of heat on moisture levels. Research indicates that dehydration in elderly nursing home residents was identified in 50-90% of cases, highlighting the urgency of proactive hydration strategies.
- Create a Hydration Schedule: Establish a routine for consuming beverages, such as having a glass of water with each meal and snack. This organized approach can assist in ensuring that seniors achieve their daily hydration targets, which should be approximately 1.6 liters for senior women and 2.0 liters for senior men, as suggested by the ESPEN guidelines.
- Use Flavor Enhancers: If plain water is unappealing, consider adding flavor enhancers or offering herbal teas to promote beverage intake. Research shows that flavored drinks can greatly enhance fluid consumption among older individuals, making staying hydrated a more enjoyable experience. As noted by Ana Reisdorf, “Functional waters, jellies, and juices containing nutrients such as proteins and minerals offer the highest moisture advantage per ounce.”
By applying these thoughtful strategies, we can greatly improve fluid levels and overall well-being in seniors, helping to decrease the risk of complications associated with dehydration in elderly. Regular assessments of hydration status and adjustments to these strategies based on individual needs are essential for effective hydration management. Remember, your comfort and health are our priority, and we’re here to support you every step of the way.
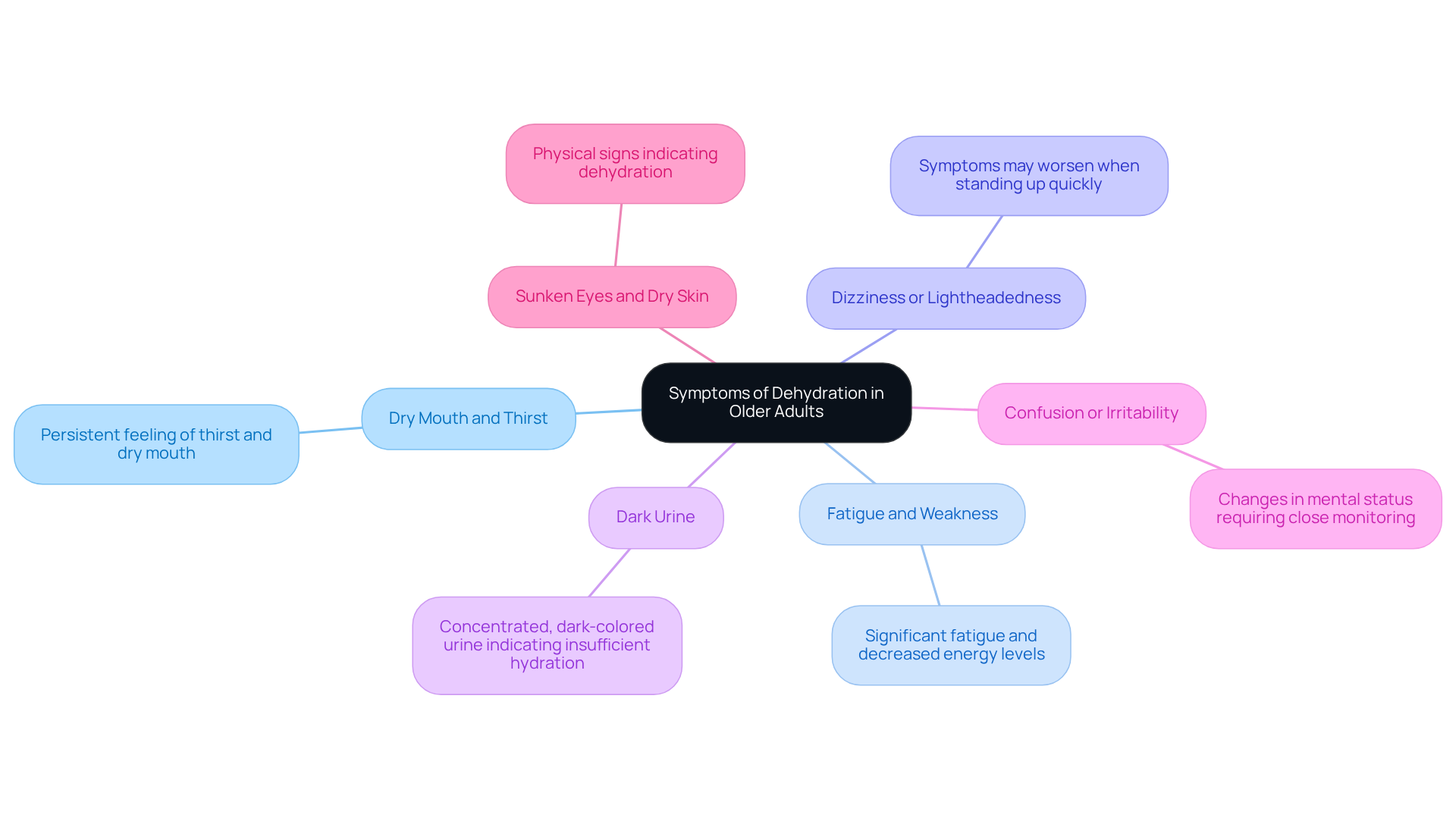
Recognize Symptoms of Dehydration in Older Adults
Identifying the signs of dehydration in elderly individuals is essential for prompt action. As caregivers, it’s important to be aware of the common signs that can indicate dehydration:
- Dry Mouth and Thirst: A persistent feeling of thirst and a dry mouth are often the first indicators of dehydration. Many older adults may not recognize these early signs of dehydration in elderly individuals, which can lead to further complications.
- Fatigue and Weakness: Dehydration can result in significant fatigue and decreased energy levels, making daily activities more challenging.
- Dizziness or Lightheadedness: These symptoms may manifest, particularly when standing up quickly, and can be exacerbated by dehydration in elderly, increasing the risk of falls.
- Dark Urine: Concentrated, dark-colored urine is a strong indicator of insufficient hydration, which may contribute to dehydration in elderly individuals, signaling that the body is not receiving adequate fluids.
- Confusion or irritability can indicate dehydration in the elderly, highlighting the need for caregivers to monitor mental status closely.
- Sunken Eyes and Dry Skin: Physical signs like sunken eyes and dry, flaky skin may also be present, indicating dehydration in elderly individuals and a need for immediate hydration.
Statistics indicate that dehydration in elderly affects 20-30% of senior citizens, frequently resulting in higher mortality and morbidity rates. For example, a study revealed that 37% of senior adults were experiencing dehydration in elderly upon hospital admission, with nearly two-thirds still being dehydrated 48 hours later. Recognizing these symptoms early can lead to prompt treatment for dehydration in elderly and significantly improve health outcomes.
As noted by geriatric clinical nurse specialists, “Many people aged 65 and older don’t drink enough liquids,” and “by the time an older adult feels thirsty, that’s already an indication of early dehydration.” This emphasizes the importance of awareness and proactive monitoring among caregivers. Remember, we’re here for you, and your comfort is our priority.
Conclusion
Dehydration in elderly individuals is a significant health concern that requires our attention and proactive measures. By acknowledging the unique challenges faced by seniors—such as diminished thirst response, chronic illnesses, and mobility issues—caregivers can play a vital role in ensuring adequate hydration. The consequences of dehydration extend beyond mere discomfort; they can lead to serious health complications, including cognitive decline and increased hospitalization rates.
Throughout this article, we explored various causes of dehydration, highlighting the importance of monitoring fluid intake and recognizing symptoms early. Key strategies for prevention include:
- Encouraging regular hydration
- Offering hydrating foods
- Creating structured drinking schedules
These strategies can truly make a difference in the lives of older adults. We encourage caregivers to remain vigilant and supportive, as even minor adjustments can significantly enhance the quality of life for seniors.
Ultimately, the responsibility lies with all of us to prioritize hydration for our elderly loved ones. By understanding the risks and implementing effective strategies, we can help ensure that seniors remain healthy and vibrant. Taking action now not only safeguards their well-being but also fosters a more compassionate and supportive environment for our aging population. Remember, we’re here for you, and your comfort is our priority.
Frequently Asked Questions
What is dehydration and how does it affect the elderly?
Dehydration occurs when the body loses more fluids than it takes in, leading to insufficient water and electrolytes necessary for normal bodily functions. It is particularly concerning for the elderly, who may be at higher risk due to reduced thirst sensation, medications that promote fluid loss, and various health conditions.
What percentage of elderly individuals are affected by dehydration?
Recent studies indicate that dehydration affects 20% to 30% of older adults.
What are some serious complications associated with dehydration in the elderly?
Serious complications from dehydration in elderly individuals can include urinary tract infections, kidney stones, and increased hospitalization rates. Insufficient hydration can also double the mortality rate among stroke patients.
What are the cognitive and physical effects of chronic fluid deficiency in older adults?
Chronic fluid deficiency can lead to cognitive decline, mood changes, and physical complications such as falls and fractures.
How can caregiver services help prevent dehydration in elderly individuals?
Caregiver services, such as those provided by CNA/HHA caregivers, help monitor fluid intake, assist with meal preparation for proper nutrition, and support personal hygiene, which are all essential in preventing dehydration in elderly individuals.
Why is it important to ensure proper hydration in elderly individuals?
Ensuring proper hydration is vital for safeguarding the well-being and quality of life of older adults, as it helps prevent serious health complications and enhances their overall health outcomes.











